Foot Complications in Diabetes
Diabetes is a chronic metabolic disorder occurring when there is an increase in blood glucose level, because the body is unable to produce enough insulin or cannot utilize the insulin already produced. It is the most common non-communicable disorder increasing at an alarming rate.
According to the International Diabetes Federation approximately 463 million people were reported to have diabetes in 2019 and by 2045 this number will rise to 700 million worldwide. India has the second largest number of individuals suffering from diabetes reported with a count of 77 million.
Generally, it is classified as Type 1 (insulin deficient) & Type 2 (insulin resistance) Diabetes Mellitus. The World Health Organization (WHO) recommends oral blood glucose testing for its diagnosis. This disorder is managed by medications such as insulin, oral hypoglycemic agents and lifestyle modifications including diet and exercises. But if neglected, it can cause several complications and can be fatal ,if left untreated.
Diabetes is a multi organ disorder, affecting eyes, heart, kidneys, blood vessels, and nerves. Long-term complications of diabetes develop gradually. The longer you have diabetes — and the less controlled your blood sugar — the higher the risk of complications. Possible complications include:
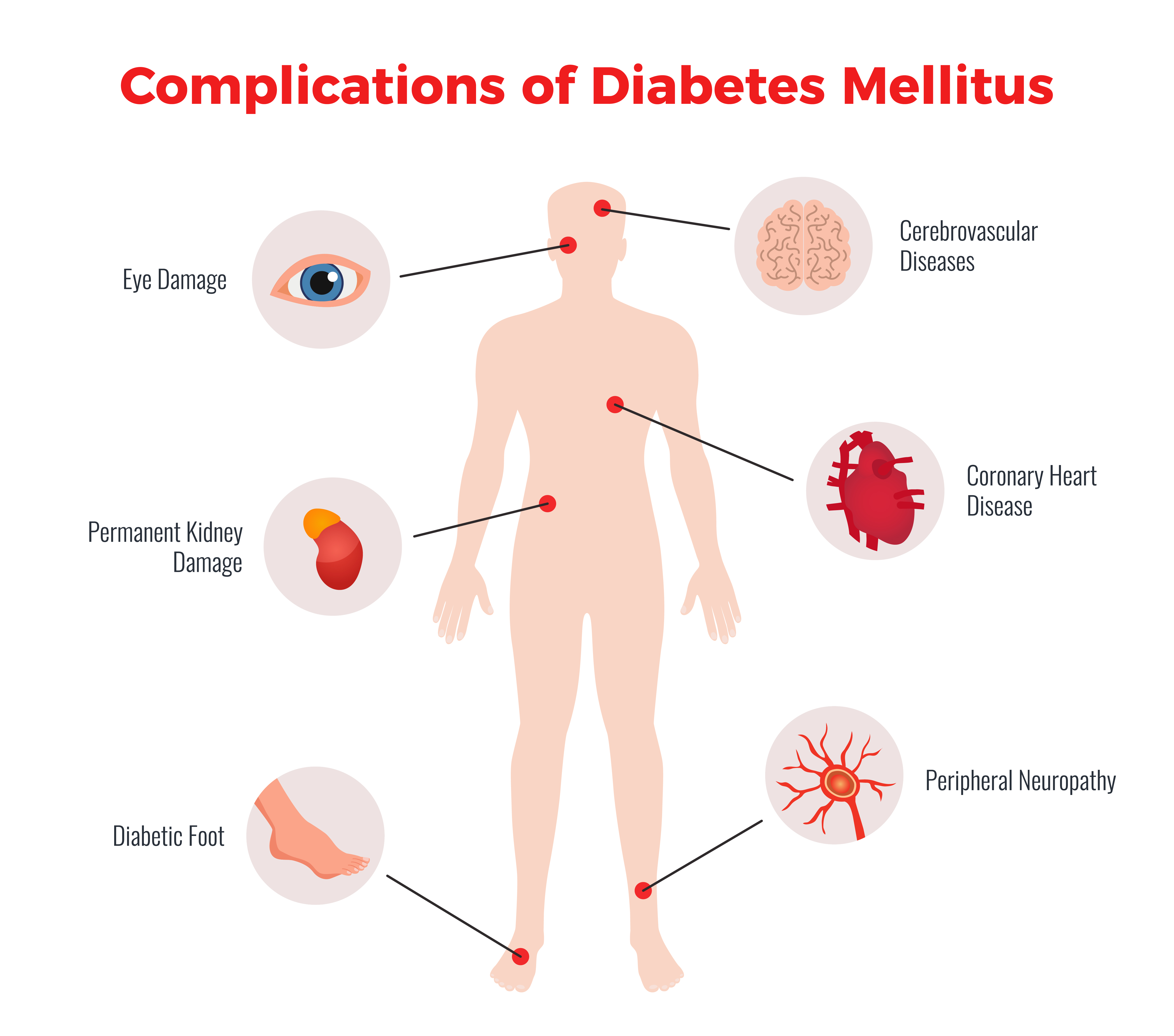
Out of all the complications Diabetic foot is one of the most significant and disabling complications of diabetes.
Diabetic Foot
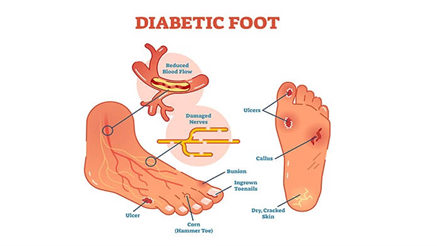
According to the WHO, Diabetic foot is characterized as a classical triad of neuropathy, ischemia, and infection which results in the formation of corns, calluses on the plantar surface of the foot further causing ulceration and deep tissue injuries. It is one of the reasons for long-stay hospitalization. It accounts for the highest number of non-accidental amputations resulting in a high rate of disability. Hence, preventing diabetic foot should be the first priority.
This can be achieved by identifying high-risk individuals, like those with peripheral neuropathy, peripheral vascular disease, ulcers, and foot deformities.
Diabetic foot ulcers:
An ulcer is a sore in the skin that may enter the bone tissues. Because of Angiopathy and neuropathy in the feet, cuts or blisters can easily turn into ulcers that become infected and will not heal.
Ulcers occur most often on the ball of the foot or on the bottom of the big toe. Ulcers on the sides of the foot are usually due to poorly fitting shoes. Even though some ulcers do not hurt, every ulcer should be seen by your healthcare provider right away. Neglecting ulcers can result in infections, which in turn can lead to loss of a limb.
Corns and Calluses:
Corns and calluses are hard, thickened areas of skin on an area of the body that develops as a response to constant irritation, pressure or friction. The body forms a layer of hardened skin around the areas that face constant friction to protect the skin layers deep inside.
A callus is an area of rough, thick skin that forms on the balls or heels of your feet. A callus is not painful and is usually much bigger than corn.
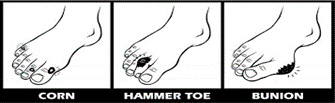
A corn is a kind of callus with a hard center and it is encircled by an area of inflamed skin. They are often painful. They are seen on weight-bearing areas, like tops and sides of the toes and in between them.
Hammertoes and Bunions:
Damage to blood vessels and nerves, ligament laxity, and muscle imbalance in the foot, causes a toe bending deformity, called hammertoe. Due to all these factors, blood flow to the muscles is reduced leading to muscle mass loss and joint stiffness. There is visible bending of the toe appearing like a hammer. Due to constant weight-bearing while standing, walking or other activities these deformities lead to ulcer formation on the foot with sensory loss.
Charcot Foot:
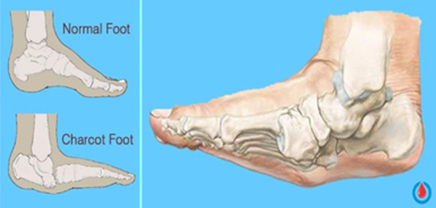
This is a complex foot deformity. It is an interaction of diabetes, neuropathy, and trauma resulting in loss of sensation and an undetected broken bony structure that leads to the destruction of the soft tissue of the foot. People with diabetes suffer from sensory loss, thus causing the pain of the fracture going unnoticed and the patient continues to walk on the broken bone, with undetected injury or irritation. In Charcot's foot, midfoot is involved leading to the collapse of the arch and giving it the appearance of rocker at the bottom. Hence, also called a rocker-bottom foot, In addition, neuropathic patients with a tight Achilles tendon (calf muscles) have been shown to have a tendency to develop Charcot foot. This disabling complication is so severe that surgery, and occasionally amputation, may become necessary.
Diabetes lowers the amount of blood flow in the feet. Not having enough blood flowing to the legs and feet can make it hard for a wound to heal. An infected wound might lead to gangrene. Gangrene and ulcers that do not get better with treatment or the damage are irreparable, amputation may be necessary. The most common amputations in people with diabetes are the toes, feet, and lower legs.
Because of its seriousness, it is important that people living with diabetes take preventive measures and seek immediate care if signs or symptoms appear.
Prevention is better than Cure...Delay can lead to serious health complications. Hence, manage your diabetes and keep your feet healthy to have a healthy lifestyle.